
A recent Part B News article has highlighted RPM revenue codes provided by CMS. These various codes can become a revenue opportunity for a practice.
Providers are taking a cautious jump into a suite of remote monitoring and virtual evaluation services that Medicare has approved for use in recent years, but the early returns reveal significant revenue possibilities.
Among a series of three remote patient monitoring codes – 99453, 99454 and 99457 – that debuted in 2019, providers topped out at 61,766 claims for 99454, a service that records and tracks a patient’s health metrics remotely. Despite the relative slow rate of adoption, providers were rewarded with nearly $3 million in payments for the virtual care code.
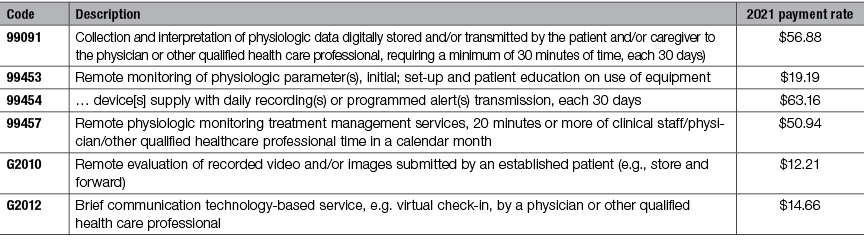
Practices reported remote monitoring management services code 99457 nearly 59,000 times in 2019, bringing in $2.2 million in Medicare reimbursement, according to the latest available Medicare claims data. Third on the list was remote monitoring set-up code 99453 with 22,000 claims and $319,000 in payments.
A fourth remote monitoring code, 99091, which gained active status in 2018, showed worrying signs in its second year of use. While claims rose at a 26% rate between 2018 and 2019, the code’s denial rate skyrocketed from just shy of 10% to more than 29%. That climb in denials held total payments in check, reaching $1.3 million in 2019 – just a 3% rise in payments from year to year.
Providers were less likely to dive into a pair of virtual patient care codes, remote evaluation service G2010 and virtual check-in service G2012. In 2019, practices reported 12,426 claims for G2012, which pays about $15 per claim. The G2010 store-and-forward service totaled 961 claims, netting $10,677 in payments.
We believe that RPM is a key service opportunity for patients today and in the future. You can expect private payers to follow the lead of CMS going forward. RPM provides access to care, real-time monitoring, lowers the cost of care and improves the quality of life for patients.
